Part 1: The physiology of transition ( Embrionic > Fetal > transition > Neonatal (Newborn )
 >
>  < fetus to neonate >
< fetus to neonate > 
:: Neonatal Cardiovascular System Diagram ( larger )
HOME date: 9-9-2020 --- about the human birth event - in 2020 - the Science :::
Note: I am a senior, retired American - and made this page because the subject interest me. I am NOT pregnant. - My grown daughter is an attorney.
https://embryology.med.unsw.edu.au/embryology/index.php/Embryonic_Development
https://en.wikipedia.org/wiki/Epithelial_sodium_channel
SOURCE: https://acutecaretesting.org/en/articles/fetaltoneonatal-transition-what-is-normal-and-what-is-not-part-1
( Content hyperlinked by Susan - and "enhanced" for my personal understandin)
July 2007 :: " Fetal-to-neonatal transition: What is normal and what is not? Part 1"
by Debbie Fraser Askin : more : " Neonatology Blood gases/acid-base Glucose "
https://acutecaretesting.org/en/about/contact :: Attn.: Acutecaretesting.org Editorial Team, Åkandevej 21, 2700 Brønshøj, Denmark ::
EMAIL acutecaretesting@radiometer.net
9-9-2020
acutecaretesting@radiometer.net
Dear Ms. Askin (Author). My name is Susan Neuhart. I am a retired American. Now retired, I suffered a SAH@MCA event. My stroke rehabilitation - from this "medical event" - requires physical and mental practices. Thus, I perform YOGA poses (daily) AND have a "personal" web site - "HTML" - for mental stimulation - etc.
Now, I have "drafted" an "HTML" web page - at my site - https://hansandcassady.org/birth.html - which, utilizes your "published" content. I cite you as the "source". THANK YOU FOR THE INTERESTING INFORMATION!
I enhanced it - for my own understanding. I attended College (UWGB) with "nursing students" - however, I am a retired software professional. My husband is a Medical & Scientific Illustrator: https://www.sciencevectorart.com/
HOWEVER, it has come to my attention - the majority of the 22 "references" you cite - in your article - require a "purchase" - to view them. [ https://hansandcassady.org/birth.html ] As your physical address is Denmark (country of) - you may not be aware [this] is considered very bad form - in America. That is, specifically - to publish scientific - research - information - which appears to be referenced (to legitimate scientific sources) - and then, require the "End User" (a person such as me) to "purchase access" - to verify or consult the cited source. I wanted to make you aware [that] your "editors" [I presume you have them] - have made this mistake - as described above.
Please note, the creation of "Journal" information (research information) - in America - using "tax payer money" - and, then - locking the "results" behind a "purchase access gate" - is about to become a significant portion of the American US Election NEWS cycle. SEE letter to US President Donald Trump from Journal Owners, representatives, etc. at end - of cited HTML page a .
Please notify me - if you decide to update your cited references. You may realize [that] you can do this with a "pass key" technique - which, the Journals can supply - the details.
Thank you. - Susan ( Please access my "HOME" page - to find out "about" me - if required. Again, I am "retired". )
Part 1: The physiology of transition ( Embrionic > Fetal > transition > Neonatal (Newborn )
 >
>  < fetus to neonate >
< fetus to neonate > 
:: Neonatal Cardiovascular System Diagram ( larger )
The transition from fetus to neonate is a critical time of physiological adaptation.
While the majority of term [human] infants complete this process in a smooth and organized fashion,
some infants experience a delay in transition or exhibit symptoms of underlying disease.
{ https://www.nature.com/articles/pr200967 : "Breathing Patterns in Preterm and Term Infants Immediately After Birth" }
Careful assessment and astute care is needed during the period of transition to ensure that the neonate - who is experiencing problems with transition - is recognized and appropriate interventions initiated.
[ "... Following embryonic development the fetal stage of development takes place. ..."
[ https://en.wikipedia.org/wiki/Embryonic_development :: http://dhy104prenataldev.weebly.com/fetal-period.html ]
Part 1 of this paper examines the physiology of transition, focusing on the changes occurring in the cardiovascular and respiratory systems.
(Part 2 will address the signs and symptoms which indicate the need for further evaluation of the infant.)
The transition from fetal to neonatal life requires complex physiological changes that must occur in a relatively short period of time.
The fetus must move from reliance on the maternal heart, lungs, metabolic and thermal systems (through the placenta)
to being able to self-sufficiently deliver oxygenated blood to the tissues and regulate various body processes (as an individual).
While the majority of critical transitions occur in the first few moments after birth, circulatory and pulmonary changes continue for up to 6 weeks after birth.
Transition is a time of significant risk to the newborn and necessitates astute observations on the part of the healthcare team.
While most term infants achieve physiological homeostasis without difficulty, careful assessment during this period of adaptation is required to ensure that the infant makes the transition smoothly and without compromise.
Prompt recognition of those infants who present with signs of serious illness enables caregivers to initiate treatment aimed at minimizing the effects of such illness.
This article will review the physiological adaptations occurring during the transition from fetal to neonatal life and will examine common red flags which may alert care providers to an infant experiencing delayed transition or an underlying disease process, congenital abnormality or birth injury.
PHYSIOLOGY OF TRANSITION :: Cardiovascular changes : Respiratory adaptations : Thermal and metabolic adaptation
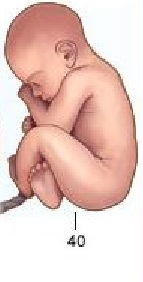
Cardiovascular changes
Fetal circulation is characterized by the presence of three shunts, the 1) ductus venosus, 2) ductus arteriosus and 3) foramen ovale, as well as high pulmonary vascular resistance (PVR) resulting from the relative hypoxic pulmonary environment ( pO2 17-19 mmHg ) and low systemic vascular resistance (SVR) [5 < bad ref. Must purchase to view].
[ related : NOAA : https://oceanservice.noaa.gov/hazards/hypoxia/ :: < low oxygen levels & "fish kills" - BOD biologic oxygen demand ] ::
Adult human > hhhh
[ https://en.wikipedia.org/wiki/Circulatory_system ]
ductus venosus :: https://en.wikipedia.org/wiki/Ductus_venosus
ductus arteriosus :: https://en.wikipedia.org/wiki/Ductus_arteriosus
foramen ovale :: https://en.wikipedia.org/wiki/Foramen_ovale_(heart)
pulmonary vascular resistance (PVR) :: https://www.ncbi.nlm.nih.gov/books/NBK554380/
hypoxic pulmonary environment (pO2 17-19 mmHg) :: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3154643/
systemic vascular resistance (SVR) :: https://www.cvphysiology.com/Blood%20Pressure/BP021
To fully appreciate the hemodynamic changes which occur after birth, a review of fetal circulation is necessary (Fig. 1).
[ https://en.wikipedia.org/wiki/Fetal_circulation ]
FIGURE 1: Neonatal Cardiovascular System ( Reprinted by permission from Ross Labs http://www.rosslearningcenter.com/ < requires MD license to view )
 ( larger )
( larger ) 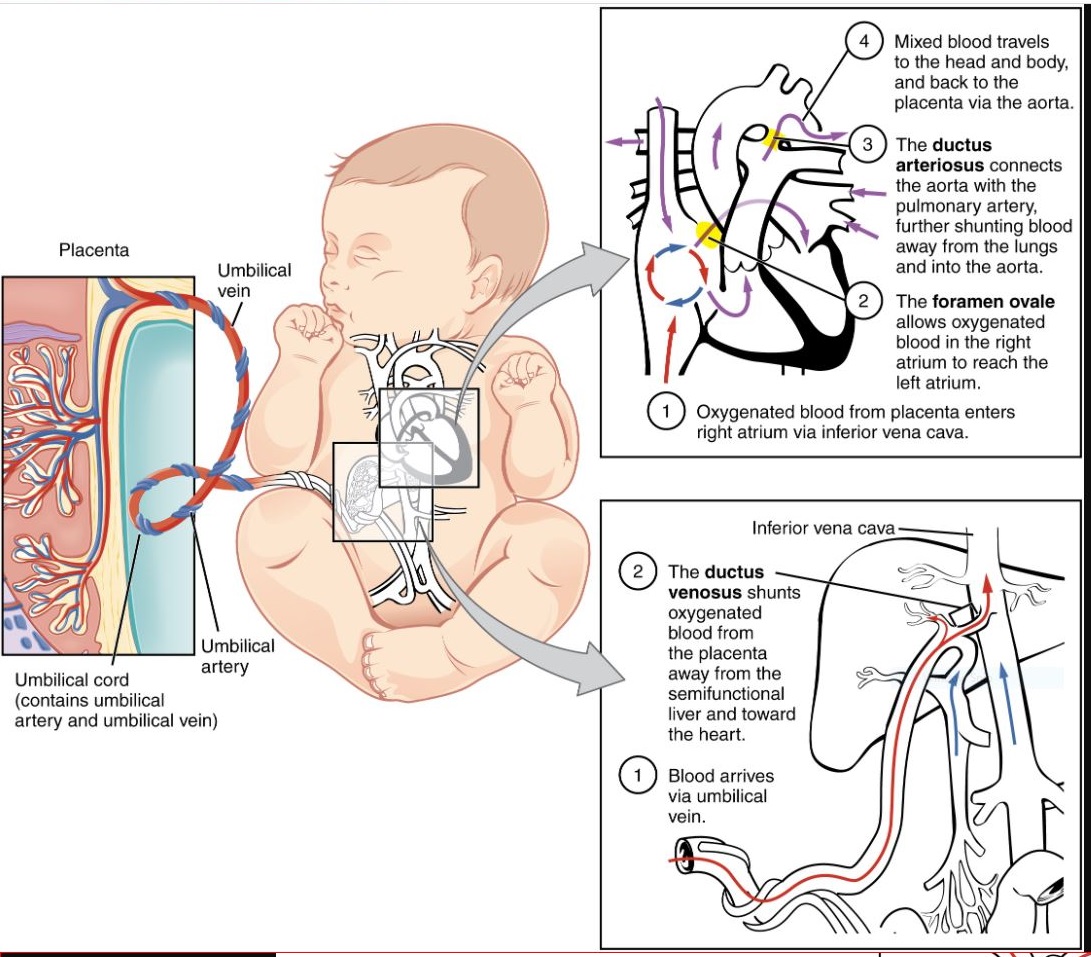 < Larger [ [SOURCE: https://en.wikipedia.org/wiki/Fetal_circulation ]
< Larger [ [SOURCE: https://en.wikipedia.org/wiki/Fetal_circulation ]
SOURCE: https://acutecaretesting.org/-/media/acutecaretesting/articles/5f2ecdef-ee33-459d-b62f-0be3ae0515df.jpg?w=400&h=529&as=1
hh 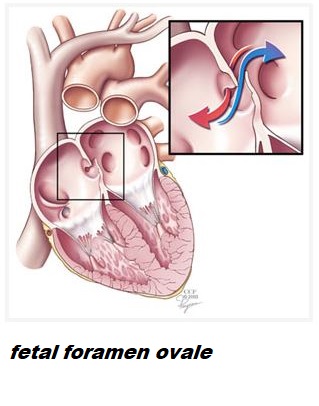
< Adult human heart
In "utero" [ a Latin term literally meaning "in the womb" or "in the uterus"] oxygenated blood is delivered from the placenta to the fetus through the umbilical vein and into the liver. Some of this blood perfuses the fetus liver, while the rest of the blood bypasses the hepatic system (image above) through the first fetal shunt, the ductus venosus, which forms a connection between the umbilical vein and the inferior vena cava (IVC). [ wikipedia : https://en.wikipedia.org/wiki/Ductus_venosus ]
The percentage of blood directed towards the fetus liver increases with increasing gestational age with about 80 % entering the liver by 32 weeks' gestation [3,14,15].
In the Inferior Vena Cava (IVC) oxygenated blood from the ductus venosus mixes with unoxygenated blood from the lower body although the oxygenated blood, which has a higher level of kinetic energy, tends to remain in a relatively separate stream [5].
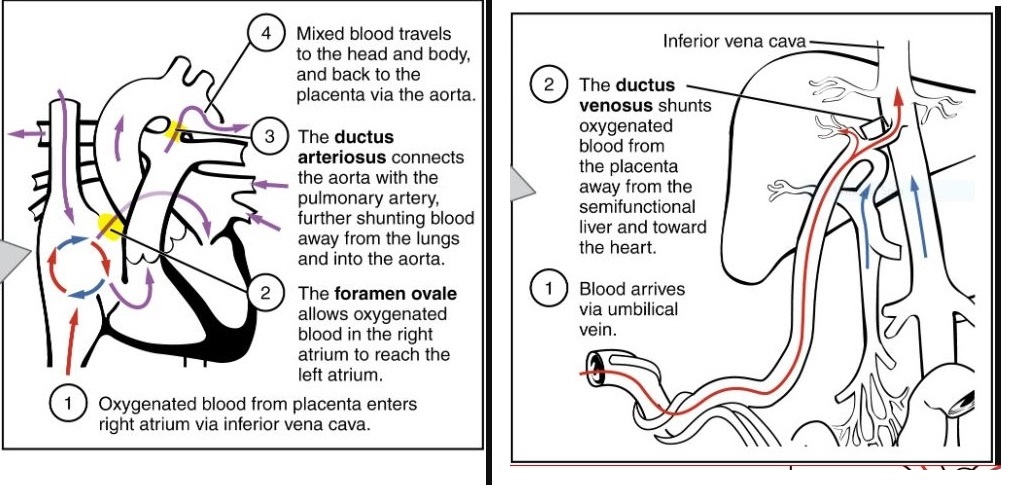
When the stream of oxygenated blood enters the right atrium, about 50-60 % is directed through the foramen ovale to the left atrium by the Eustatian valve (a flap of tissue at the IVC right-atrium junction) [5].
The foramen ovale is ... a flaplike structure between the right and left atria that acts like a one-way valve.
h 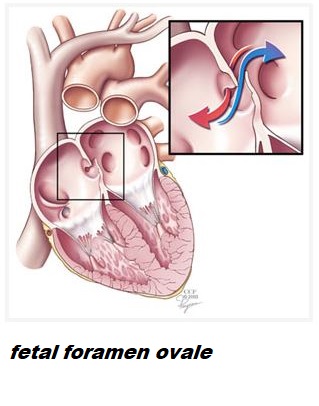 Adult human heart diagram>
Adult human heart diagram>
"... What is the Foramen Ovale? :: The foramen ovale (foh-RAY-mun oh-VAY-lee) is a small hole located in the septum, which is the wall between the two upper chambers of the heart (atria). ...Before a baby is born, it does not use its lungs to get blood rich in oxygen. Instead, this blood comes from the mother’s placenta and is delivered through the umbilical cord. The foramen ovale makes it possible for the blood to go from the veins to the right side of the fetus’ heart, and then directly to the left side of the heart. ... The foramen ovale normally closes as blood pressure rises in the left side of the heart after birth. Once it is closed, the blood flows to the lungs to get oxygen before it enters the left side of the heart and gets pumped to the rest of the body. ..." [ SOURCE: https://my.clevelandclinic.org/health/diseases/17326-patent-foramen-ovale-pfo ]
Blood flows across (AND through) the foramen ovale because high pulmonary vascular resistance maintains pressure in the right atrium at a level greater than that of the left atrium.
The superior vena cava drains deoxygenated blood from the head and upper extremities into the right atrium, where it mixes with oxygenated blood from the placenta.
This blood enters the right ventricle and pulmonary artery where, again, increased resistance in the pulmonary vessels causes 90 % of this blood to be shunted across the ductus arteriosus and into the aorta.
This mixture of oxygenated and deoxygenated blood continues through the descending aorta and eventually drains back to the placenta through the umbilical arteries. ( above MAIN illustration larger )
The remaining 10 % the blood coming from the right ventricle perfuses the lung tissue to meet metabolic needs. The blood that actually reaches the lungs represents about 8 % of the fetal cardiac output [10,4].
After 30 weeks of gestation the amount of blood perfusing the lungs gradually increases in preparation for birth [5].
During fetal life, the placenta is an organ of low vascular resistance.
Clamping the umbilical cord at birth eliminates the placenta as a reservoir for blood, causing a rise in blood pressure and SVR. [ "delayed" ]
As oxygen enters the lungs [at birth] , the pulmonary vascular bed dilates, increasing blood flow to the lungs and causing pressure in the right atrium to fall.
[ https://my.methodistcollege.edu/ICSFileServer/eaab96b1-8b9c-444b-9085-16793ddf084a/c71ed1f1-4f9f-403e-9035-872974270971/da419c5e-75b1-448d-b688-7d9beced2663/ONL177/ONL177_print.html < GOOD ARTWORK - DIAGRAMS ]
The increased pulmonary venous return to the left atrium and less blood flow into the right atrium cause the left atrial pressure to exceed the pressure in the right atrium, resulting in functional closure of the foramen ovale [12].
After closure, blood is directed from the right atrium to the right ventricle and on to the lungs - rather than through the foramen ovale.
Shunting of blood from the pulmonary artery through the ductus arteriosus to the aorta occurs as a result of high PVR.
After birth, SVR. rises and PVR falls, causing a reversal of blood flow through the ductus [? arteriosus ?] and an 8-10 fold increase in pulmonary blood flow [4].
In utero, patency of the ductus arteriosus is maintained by high levels of prostaglandins and the low fetal pO2.
Prostaglandins are secreted by the placenta and metabolized in the lungs.
Smaller volumes of blood passing through the fetal lungs result in elevated circulating prostaglandins levels which fall after birth as more blood flows to the lungs [5].
The major contributing factor to closure of the ductus arteriosus is sensitivity to rising arterial oxygen concentrations in the blood [6].
As the pO2(aB) level increases after birth, the ductus arteriosus begins to constrict.
Removal of the placenta decreases prostaglandin levels, further influencing closure [13,1].
Constriction of the ductus arteriosus is a gradual process, permitting bidirectional shunting of blood after birth.
PVR may be higher than the SVR, allowing some degree of right-to-left shunting, until the SVR rises above PVR and blood flow is directed left to right.
Most neonates have a ... ( patency of the ductus arteriosus ) in the first 8 hours of life with spontaneous closure occurring in 42 % at 24 hours of age, in 90 % at 48 hours of age and in almost all infants at 96 hours [9,12].
Permanent anatomic closure of the ductus arteriosus occurs within 3 weeks to 3 months after birth.
Prior to birth the pulmonary blood vessels have a thick layer of smooth muscle, which plays a key role in pulmonary vasoconstriction.
After birth this muscle layer becomes less sensitive to changes in oxygenation and begins to thin, a process which continues for 6-8 weeks [17].
Any clinical situation that causes hypoxia, with pulmonary vasoconstriction and subsequent increased PVR, potentiates right-to-left shunting across the ductus arteriosus and foramen ovale [18].
When the umbilical cord is clamped, blood flow through the umbilical vein to the ductus venosus ceases.
Systemic venous blood flow is then directed through the portal system for hepatic circulation. Umbilical vessels constrict, with functional closure occurring immediately. Fibrous infiltration leads to anatomic closure in the first week of life in term infants [1].
Respiratory adaptations
At birth the clamping of the umbilical cord signals the end of the flow of oxygenated blood from the placenta.
To establish effective ventilation and tissue oxygenation, the neonate must clear the lungs of fetal lung fluid, establish a regular pattern of breathing and match pulmonary perfusion to ventilation.
Other factors, including pulmonary blood flow, surfactant production and respiratory musculature also influence respiratory adaptation to extrauterine life.
In utero, the lung epithelium secretes fluid, a process which is essential to the normal growth and development of the alveoli [22].
Toward the end of gestation, the production of lung fluid gradually diminishes and absorption of fluid begins.
A complete understanding of this process is still lacking but some theories have emerged from work on fetal lambs suggesting that sodium reabsorption plays a key role [11].
The catecholamine surge that occurs just before the onset of labor has also been shown to correspond to a more rapid drop in fetal lung fluid levels [16,19].
Those infants who do not experience labor, such as those born by elective cesarean section, are more likely to have residual fluid in the lungs and develop Transient Tachypnea of the Newborn (TTN) because of lower levels of serum catecholamine [11].
Initiation of breathing is a complex process that involves the interplay of biochemical, neural and mechanical factors, some of which have yet to be clearly identified [1].
A number of factors have been implicated in the initiation of postnatal breathing: decreased oxygen concentration, increased carbon dioxide concentration and a decrease in pH, all of which may stimulate fetal aortic and carotid chemoreceptors, triggering the respiratory center in the medulla to initiate respiration.
Some researchers have questioned the influence of these factors and suggest instead that factors secreted by the placenta may inhibit breathing, and that regular breathing is initiated with the clamping of the cord [1]. [ "delayed clamping of the cord" ]
Mechanical compression of the chest creates negative pressure and drawing air into the lungs as the lungs re-expand.
Further expansion and distribution of air throughout the alveoli occur when the newborn cries.
Crying creates a positive intrathoracic pressure that keeps alveoli open and forces the remaining fetal lung fluid into pulmonary capillaries and the lymphatic circulation.
Thermal and metabolic adaptation
The core temperature of the fetus is typically about 0.5 °C above that of the mother and therefore the fetus expends no energy staying warm [20].
After birth the newborn’s ability to maintain temperature control is determined both by environmental factors and internal physiological processes.
Newborns are predisposed to heat loss because of factors such as: a large surface area in relation to body weight, limited body fat and a decreased ability to shiver [2].
Newborns attempt to stay warm by increasing muscle activity and by burning brown fat (non-shivering thermogenesis), which increases metabolic rate.
Peripheral vasoconstriction also decreases heat loss to the skin surface.
The production of heat requires oxygen and glucose and produces lactic acid; therefore persistent hypothermia may result in metabolic acidosis, hypoglycemia, decreased surfactant production, and over the longer term, poor growth [2].
Maternal glucose readily crosses the placenta and, under normal circumstances, supplies the fetus with enough energy to grow appropriately and to store glycogen in the liver for use after birth.
The release of catecholamines occurring during labor and birth mobilizes glycogen; however, blood glucose levels decline after birth, reaching their lowest point at 1 hour of age [21].
NORMAL TRANSITIONAL FINDINGS
Much of the work of transition is accomplished in the first 4-6 hours following delivery, while final completion of the cardiovascular changes may take up to 6 weeks [5].
During the initial hours after birth, the majority of fetal lung fluid is reabsorbed, a normal functional residual capacity is established in the lungs and the cardiovascular system redistributes blood flow to the lungs and tissues.
The infant moves through a fairly predicable series of events mediated by the sympathetic nervous system that results in changes in heart rate, respirations, gastrointestinal function and body temperature.
In a classic description still used today, Desmond and colleagues [7] organized these changes into three stages:
1. The first period of reactivity (0-30 minutes) characterized by an increase in heart rate, irregular respirations and fine crackles in the chest with grunting and nasal flaring
2. A period of decreased responsiveness (30 minutes to 3 hours) with rapid shallow respirations, lower heart rate, decreased muscle activity interspersed with jerks and twitches and sleep
3. A second period of reactivity (2-8 hours) in which exaggerated responsiveness, tachycardia, labile heart rate, abrupt changes in tone and color, and gagging and vomiting are commonly seen [7]
Residual symptoms of transition such as crackles in the lungs, a soft cardiac murmur and acrocyanosis may persist for periods of up to 24 hours in otherwise healthy infants [8].
SUMMARY
The majority of newborns complete the process of transition with little or no delay. These infants may demonstrate normal transitional findings, including tachypnea and tachycardia, a soft heart murmur and fine crackles in the lungs as well as acrocyanosis for varying lengths of time after birth. Prolonged or exaggerated signs of distress should lead the healthcare provider to carry out a thorough physical examination and review of the maternal and newborn history to establish the etiology of the symptoms. This will allow the rapid initiation of appropriate interventions aimed at minimizing the morbidity resulting from problems of transition or underlying diseases processes. Part 2 of this series will examine signs and symptoms that may assist the healthcare team identify the infant in need of further evaluation during the period of transition.
...
Acutecaretesting.org is part of Radiometer. [ https://www.radiometeramerica.com/ ]
1. Alvaro RE, Rigatto H. Cardiorespiratory adjustments at birth. In: Avery’s neonatology pathophysiology & management of the newborn. 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2005: 285-303.
2. Askin DF. Complications in the transition from fetal to neonatal life. J Obstet Gynecol Neonatal Nurs 2002; 31(3): 318-27.
3. Bellotti M, Pennati G, De Gasperi C, Battaglia FC, Ferrazzi E. Role of ductus venosus in distribution of umbilical blood flow in human fetuses during second half of pregnancy. Am. J. Physiol Heart Circ Physiol 2000; 279(3): H1256-63.
4. Blackburn ST. Maternal, fetal, & neonatal physiology. A clinical perspective. Philadelphia: Saunders, 2003.
5. Blackburn S. Placental, fetal and transitional circulation revisited. Journal of Perinatal & Neonatal Nursing 2006; 20(4): 290-4. [ must purchase ]
6. Clyman RI. Mechanisms regulating closure of the ductus arteriosus. In: Polin RA, Fox WW, Abman SH, eds. Fetal neonatal physiology. Philadelphia: Saunders, 2004.
7. Desmond MM, Rudolph AJ, Phitaksphraiwan P. The transitional care nursery. A mechanism for preventive medicine in the newborn. Pediatr Clin North Am 1966; Aug; 13(3): 651-68. [ must purchase ]
8. Gardner SL, Johnson JL. Respiratory diseases. In: Merenstein GB, Gardner SL, eds. Handbook of neonatal intensive care. 6th ed. St. Louis: Mosby Elsevier, 2006: 79-121. [ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6110042/ ] [ must purchase ]
9. Gentile R, Stevenson G, Dooley T et al. Pulsed Doppler echocardiographic determination of time of ductal closure in normal newborn infants. J Pediatr 1981; 98: 443-448. [ must purchase ]
10. Grant DA. Ventricular constraint in the fetus and newborn. Can J Cardiol 1999; 15 (1): 95-104.
11. Jain L, Eaton DC. Physiology of fetal lung fluid clearance and the effect of labor. Seminars in Perinatology, 2006; 30: 34-43.
12. Johnson BA, Ades A. Delivery room and early postnatal management of neonates who have prenatally diagnosed congenital heart disease. Clin Perinatol 2005; 32: 921-946.
13. Kenner C. Resuscitation and stabilization of the newborn. In: Kenner C, Lott JW, (eds). Comprehensive neonatal nursing: a physiologic perspective. 3rd ed. Philadelphia: Saunders, 2003: 210-27.
14. Kiserud T, Acharya G. The fetal circulation. Prenat. Diagn 2004; 24(13): 1049-59.
15. Kiserud T, Rasmussen S, Skulstad S. Blood flow and the degree of shunting through the ductus venosus in the human fetus..Am J Obstet Gynecol 2000; 182(1 Pt 1): 147-53.
16. Lagercrantz H, Bistoletti P. Catecholamine release in the newborn infant at birth. Pediatr Res 1977; 11(8): 889-93.
17. Lakshminrusimha S, Steinhorn RH. Pulmonary vascular biology during neonatal transition. Clin Perinatol 1999; 26(3): 601-19. [ must purchase ]
18. Lott JW. Assessment and management of the cardiovascular system. In: Kenner C, Lott JW, eds. Comprehensive neonatal nursing: a physiologic perspective 3rd ed. Philadelphia: W.B. Saunders, 2003: 376-408. [ must purchase ]
19. Pfister RE, Ramsden CA, Neil HL et al. Volume and secretion rate of lung liquid in the final days of gestation and labour in the fetal sheep. J Physiol 2001: 535(3): 889-99.
20. Rutter N, Hull D. Response of term babies to a warm environment. Arch Dis Child 1979; 54(3): 178-83.
21. Sinha SK, Donn SM. Fetal-to-neonatal maladaptation. Semin Fetal Neonatal Med 2006; 11(3): 166-73.
22. Strang LB. Fetal lung fluid: secretion and reabsorption. Physiol Rev 1991; 71: 991-1016.
[end]
Conduct research with tax payer money then publish in journals that require subscription < GOOGLE > [ Bayh - Dole law ]
December 18, 2019
President Donald J. Trump
The White House
1600 Pennsylvania Avenue NW
Washington, D.C. 20500
Dear President Trump:
The undersigned organizations represent the leading publishers and non-profit scientific societies
in the United States. We write to you with deep concern regarding a proposed policy that has
come to our attention that would jeopardize the intellectual property of American organizations
engaged in the creation of high-quality peer-reviewed journals and research articles and would
potentially delay the publication of new research results. The role of the publisher is to advance
scholarship and innovation, fostering the American leadership in science that drives our
economy and global competitiveness. As copyrighted works, peer-reviewed journal articles are
licensed to users in hundreds of foreign countries, supporting billions of dollars in U.S. exports
and an extensive network of American businesses and jobs. In producing and disseminating these
articles, we make ongoing competitive investments to support the scientific and technical
communities that we serve.
As noted above, we have learned that the Administration may be preparing to step into the
private marketplace and force the immediate free distribution of journal articles financed and
published by organizations in the private sector, including many non-profits. This would
effectively nationalize the valuable American intellectual property that we produce and force us
to give it away to the rest of the world for free. This risks reducing exports and negating many of
the intellectual property protections the Administration has negotiated with our trading partners.
We write to express our strong opposition to this proposal, but in doing so we want to underscore
that publishers make no claims to research data resulting from federal funding.
To be clear, publishers both support and enable “open access” business models and “open data”
as important options within a larger framework that assumes critical publisher investments
remain viable. Under a legacy regulation that is still in force today, proprietary journal articles
that report on federally funded research must be made available for free within 12 months of
publication. This mandate already amounts to a significant government intervention in the
private market. Going below the current 12 month “embargo” would make it very difficult for
most American publishers to invest in publishing these articles. As a consequence, it would place
increased financial responsibility on the government through diverted federal research grant
funds or additional monies to underwrite the important value added by publishing.
In the coming years, this cost shift would place billions of dollars of new and additional burden
on taxpayers. In the process, such a policy would undermine American jobs, exports, innovation,
and intellectual property. It could also result in some scientific societies being forced to close
their doors or to no longer be able to support the publication of U.S.-sponsored science that is
key to ensuring that the U.S. remains the world leader in science and technology.
In addition to financing and managing a world-leading peer review process, publishers make
extensive investments in education, research, and innovative digital platforms that advance
American competitiveness and help ensure the quality and integrity of American science.
Undermining the marketplace is unnecessary, counterproductive, and would significantly harm
the system of peer-reviewed scholarly communication that fuels America’s leadership in
research and innovation.
We urge you to oppose this proposed policy, and we look forward to working with the Administration on this matter.
Sincerely yours,
AMDA – The Society for Post-Acute and Long-Term Care Medicine
American Academy of Allergy, Asthma & Immunology
American Academy of Child and Adolescent Psychiatry
American Academy of Family Physicians
American Academy of Neurology
American Academy of Ophthalmology
American Academy of Orthopaedic Surgeons
American Academy of Otolaryngology- Head and Neck Surgery
American Academy of Pediatrics
American Academy of Physical Medicine and Rehabilitation
American Association for Anatomy
American Association for Cancer Research
American Association for Pediatric Ophthalmology and Strabismus
American Association for the Study of Liver Diseases
American Association for the Surgery of Trauma
American Association of Immunologists
American Association of Occupational Health Nurses
American Association of Physicists in Medicine
American Astronomical Society
American Cancer Society
American Ceramic Society
American Chemical Society
American College of Cardiology
American College of Emergency Physicians
American College of Neuropsychopharmacology
American College of Obstetricians and Gynecologists
American College of Physicians
American College of Radiology
American College of Rheumatology
American College of Surgeons
American Contact Dermatitis Society
American Council on the Teaching of Foreign Languages
American Counseling Association
American Dental Association
American Diabetes Association
American Gastroenterological Association
American Geophysical Union
American Geriatrics Society
American Headache Society
American Heart Association
American Institute of Aeronautics and Astronautics
American Institute of Chemical Engineers
American Oil Chemists Society
American Medical Association
American Neurological Association
American Physiological Society
American Psychiatric Association
American Psychological Association
American Sexual Health Association
American Sexually Transmitted Diseases Association
American Society for Clinical Pharmacology & Therapeutics
American Society for Biochemistry and Molecular Biology
American Society for Bone and Mineral Research
American Society for Clinical Pathology
American Society for Dermatologic Surgery Association
American Society for Histocompatibility and Immunogenetics
American Society for Investigative Pathology
American Society for Nutrition
American Society for Parenteral and Enteral Nutrition
American Society for Pharmacology and Experimental Therapeutics
American Society for Radiation Oncology
American Society for Reproductive Medicine
American Society of Agricultural and Biological Engineers
American Society of Agronomy
American Society of Anesthesiologists
American Society of Animal Science
American Society of Civil Engineers
American Society of Clinical Oncology
American Society of Cytopathology
American Society of Gene & Cell Therapy
American Society of Health-System Pharmacists
American Society of Heating, Refrigerating & Air-Conditioning Engineers
American Society of Hematology
American Society of Mechanical Engineers
American Society of Nephrology
American Society of Neurorehabilitation (ASNR)
American Society of Ophthalmic Plastic and Reconstructive Surgery
American Society of Plant Biologists
American Society of Plastic Surgeons
American Society of Transplantation
American Society of Transplant Surgeons
American Thoracic Society
American Urological Association
American Water Works Association
Association for Computing Machinery
Association for Molecular Pathology
Association for Psychological Science
Association for the Sciences of Limnology and Oceanography
Association of American Publishers
Association of Schools and Programs of Public Health
Association of Teacher Educators
Biophysical Society
Botanical Society of America
Common Ground Research Networks
Council of Medical Specialty Societies
Council of Scientific Society Presidents
Crop Science Society of America
Ecological Society of America
Elsevier
Endocrine Society
Financial Management Association
Genetics Society of America
Infectious Diseases Society of America
Institute for Operations Research and the Management Sciences
Institute of Food Technologists
Institute of Industrial and Systems Engineers
International Anesthesia Research Society
International Literacy Association
International Society for Sexual Medicine
Journal of Diabetes Science and Technology, Diabetes Technology Society
Kappa Delta Pi, International Honor Society in Education
Macmillan
McGraw-Hill Education
Milbank Memorial Fund
National Council on Family Relations
National Kidney Foundation
New England Journal of Medicine published by the Massachusetts Medical Society
Orthopaedic Research Society
Radiological Society of North America
Seismological Society of America
Shock Society
Society for Leukocyte Biology
Society for Research on Adolescence
Society for the Psychological Study of Social Issues
Society for Research in Child Development
Society of General Internal Medicine
Society of Plastics Engineers
Society of Vascular and Interventional Neurology
Soil Science Society of America
Software and Information Industry Association
The Heart Rhythm Society
The Histochemical Society
The Journal of Bone & Joint Surgery, Inc.
The Minerals, Metals & Materials Society
The Optical Society
The Triological Society
The Voice Foundation
University of Chicago Press
U.S. Chamber of Commerce
Wiley
Wolters Kluwer
Cc: The Honorable Mick Mulvaney, Director, Office of Management and Budget, Acting
Assistant to the President and Chief of Staff
The Honorable Wilbur Ross, Secretary of Commerce
The Honorable Mike Pompeo, Secretary of State
The Honorable Mark T. Esper, Secretary of Defense
The Honorable Dan Brouillette, Secretary of Energy
The Honorable Robert Lighthizer, United States Trade Representative
The Honorable Russel Vought, Acting Director, Office of Management and Budget
Joe Grogan, Assistant to the President for Domestic Policy
Larry Kudlow, Director, National Economic Council
Robert O’Brien, National Security Advisor
The Honorable Kelvin Droegemeier, Director, Office of Science and Technology Policy
The Honorable Andrei Iancu, Director, United States Patent & Trademark Office
The Honorablgee Francis Collins, Director, National Institutes of Health
The Honorable France A. Córdova, Director, National Science Foundation
The Honorable Neil Jacobs, Assistant Secretary of Commerce for Environmental
Observation and Prediction
The Honorable Vishal Amin, Intellectual Property Enforcement Coordinator